Digits:
Examine the paw closely to determine if there is any foreign material present. Spread the toes and nails apart and inspect the webbing and pads. (a.)
Palpate each digit to determine if the bones are intact and whether there is soft tissue swelling. (b.)
Extend and flex the phalangeal joints and palpate the corresponding extensor and flexor tendons to see if they relax and tighten appropriately.
Test the lateral and medial stability of each joint in extension.
* Forelimb is used as an example only.

Metatarsal Bones:
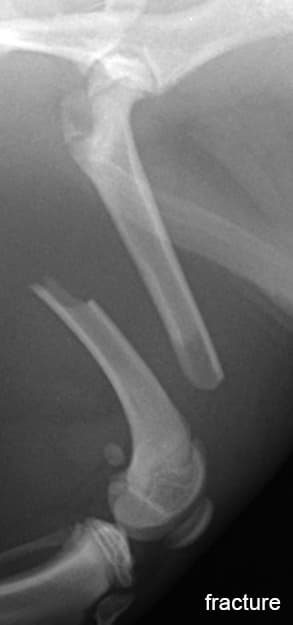
Palpate the areas adjacent to the metacarpal pad and over the palmar sesamoids of metacarpophalangeal joints 2 and 5 for sensitivity to pressure (a.). Palpate the metacarpal bones (b.) to determine if there is pain, swelling or instability (fracture).
* Forelimb is used as an example only.
Tarsus:
Palpate the tarsal joints for fluctuant swelling indicative of joint effusion.
This may be a subtle finding in the hock and is more easily noted when the animal is standing because loading the joint forces the fluid peripherally. Firm swelling is suggestive of degenerative joint disease.
Achilles Tendon:
With the stifle in extension and the hock stressed into flexion, palpate the Achilles tendon.
Rupture of the entire tendon complex allows hock flexion while the stifle is extended. Rupture of the gastrocnemius tendon and common tendon of the biceps femoris, gracilis, and semitendinosus muscles, with preservation of the superficial digital flexor, allows partial flexion of the hock while the stifle is extended and causes simultaneous flexion of the digits.
Stifle:
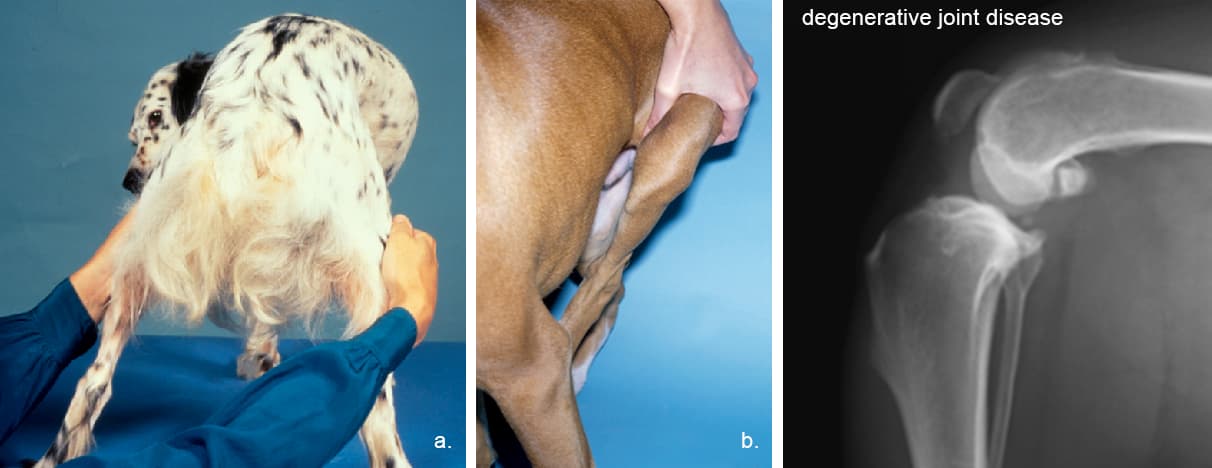
The initial perform examination of the stifle with the animal standing. Simultaneously palpate both stifles to detect swelling (a.). A swollen stifle usually indicates degenerative joint disease. The patellar ligament becomes less distinct with joint effusion and the medial aspect of the stifle enlarges because of capsular thickening and osteophyte formation (b.).
Examine the stability of the patella in relationship to the femur. Extend the stifle, internally rotate the foot, and apply digital pressure in an attempt to displace the patella medially (i.e., medial patellar luxation).
Detect lateral patellar luxation by slightly flexing the stifle, externally rotating the foot, and applying digital pressure to attempt to displace the patella laterally.
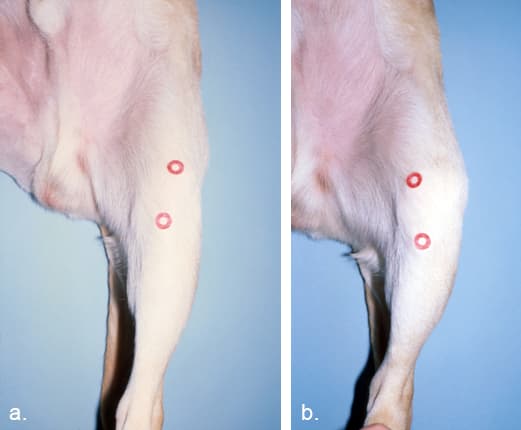
The patella (a.) normally moves slightly medially and laterally, but when it leaves the trochlear groove (b.) it is considered to be luxating.
Test the integrity of the collateral ligaments by holding the stifle in full extension and attempting to “open” the stifle on the medial and lateral aspects. Test the medial collateral ligament by using one hand to brace the femur while the other hand abducts the tibia. Normally the medial collateral ligament will not allow joint laxity.
Test the lateral collateral ligament by bracing the femur with one hand and using the other hand to adduct the tibia. An intact lateral collateral ligament will prevent joint laxity. If the stifle is allowed to flex while the tibia is adducted, it may feel as though there is lateral laxity of the joint. This is due to the anatomical location of the lateral collateral ligament and internal rotation of the tibia, and is normal.
To elicit direct drawer motion, place the index finger and thumb of one hand over the patella and lateral fabellar regions, respectively. Place the index finger of the opposite hand on the tibial tuberosity, and with the thumb positioned caudal to the fibular head, slightly flex the stifle. Stabilize the femur, and gently move the tibia cranial and distal to the femur. Do not allow tibial rotation. Tense muscles may prevent drawer motion. If tibial rotation occurs, gently flex and extend the stifle to relax the animal, and repeat the procedure.
Test drawer motion with the femur flexed and extended. Usually, the greatest movement is felt with the stifle in flexion. If the patella is luxated, replace it in the trochlear groove before attempting the drawer motion. (To view video on left, click the play button).
Minimal or partial drawer motion may also occur with incomplete tears. This drawer motion is most evident when the craniomedial band of the cranial cruciate ligament is torn. The craniomedial band must be intact to prevent drawer motion when the stifle is flexed, because the caudolateral band is relaxed at that time.
Perform the tibial compression test to detect indirect drawer motion. Detect forward motion of the tibia by placing the index finger along the patella and the tibial tuberosity.
With the leg in a standing position, flex the hock to tense the gastrocnemius muscle. This compresses the femur and tibia together causing the tibia to move forward in a cranial cruciate deficient stifle.
The presence and amount of drawer motion depends on the animal’s age, size, state of relaxation, and the duration and type of cruciate pathology. There is minimal drawer motion in normal dogs and cats, although very young puppies may have a “lax” stifle. Eliciting drawer motion in larger animals or those that are tense is difficult; sedation or general anaesthesia may be necessary.
Minimal drawer motion may be noted with chronic cruciate pathology (especially in large dogs) because periarticular fibrosis restricts stifle motion. Minimal or partial drawer motion may also occur with incomplete tears or stretching of the cranial cruciate ligament.
Drawer motion is evident with a torn caudal cruciate ligament; to identify caudal drawer motion start with the stifle in a neutral position. Most caudal ligament ruptures are not discovered until stifle exploration because they are mistaken for cranial ligament injuries.
Meniscus – In most cases, meniscal tears are identified during exploratory arthrotomy. A “click” or “pop” may be felt as the stifle is flexed and extended causing the caudal horn of the medial meniscus to displace.
Extend and flex the hip while a hand is placed over the greater trochanter to detect crepitation. The femur should extend caudally to a position almost parallel to the pelvis without inducing pain in a normal hip (a.). The stifle should approach the ilium with full flexion (b.). Degenerative joint disease limits the range of motion and may induce pain.
Hip luxation – To detect abnormalities of the hip, use the position of the greater trochanter in relationship to the tuber ischii as a landmark. In the standing animal, compare the distance from the greater trochanter to the tuber ischium bilaterally. A unilateral increase in that distance indicates hip luxation. Animals with acute hip luxations are non-weight bearing and swelling over the greater trochanter may be noted.
Externally rotate the femur while placing the thumb in the space between the greater trochanter and the tuber ischii.
Displacement of the thumb should occur.
Hip laxity – Evaluation of hip laxity is best done under sedation. With the animal in lateral recumbency, perform the Ortolani maneuver to detect hip laxity associated with hip dysplasia. Grasp the stifle with one hand and hold it parallel to the table surface. Place the other hand over the dorsal pelvis and adduct and push the stifle toward the pelvis. With joint laxity, the hip will subluxate. Maintain the pressure and abduct the stifle. As the femoral head returns to the acetabulum, use the hand stabilizing the pelvis to detect a “click”.
This procedure can also be performed with the animal in dorsal recumbency with the stifles held parallel to each other and perpendicular to the table. Apply downward pressure on the stifle to subluxate the hip. Maintain pressure and abduct the stifle. With laxity, a “click” is noted as the femoral head returns to the acetabulum.
The angle of subluxation is the point at which the hip luxates and the angle of reduction is the point at which the femoral head returns to the acetabulum.
Pelvis:
Examine the pelvic region for evidence of fracture (i.e., asymmetry, instability, swelling, crepitation, bruising, or pain). To detect instability, manipulate the tuber ischii and wings of the ilium. Radiographic evaluation is superior to physical manipulation for identifying fractures. Perform a rectal examination and note pelvic canal stenosis, pelvic fractures, and/or prostatic enlargement.